Is Addiction Market-Driven? Neurobiologist Christian Lüscher throws light on the price of pleasure
Mohit Nikalje
Tariffs and trade wars are looming threats to the global economy today, but historically, such forces have also challenged our understanding of drug addiction, showing that it is not merely a lack of self-control by an individual that causes addiction, but a more systemic problem. Disruptions to legal pharmaceutical supply chains, for instance, can create shortages fuelling illicit markets, as seen in the fentanyl epidemic.
The Opium Wars of 1839 and 1856, fought between imperial China and colonial Britain, offers one of the clearest historical examples of how trade disputes intertwine with social challenges like addiction. At its core was a trade imbalance: the British imported vast quantities of tea, silk and porcelain from China while exporting little, forcing payments in silver.
“To offset these losses, they decided to barter a commodity they produced in excess in their colonial possession, India: ‘opium’. This deliberate fuelling of mass addiction for economic gain is a prime example of how drug addiction can be market-driven,” explains Christian Lüscher, a neurobiologist and professor in the Department of Basic Neuroscience at the Faculty of Medicine, University of Geneva.
Neurobiologist Christian Lüscher
Christian, who has been studying addiction since 1999, focuses on how addictive drugs alter the brain’s communication pathways, leading to long-lasting changes in behavior and dependence. Addiction biology sparked his interest during his postdoc at the University of California, San Francisco (UCSF)
Now at the University of Geneva, he studies how addictions develop, particularly the recent menace of the “zombie drug” fentanyl and explores innovative ways to reverse them using novel methods in electrophysiology coupled with optogenetics.
How Does the Brain Learn Addiction?
The compulsive use of addictive substances is a universal problem that transcends all cultures and geographies, as do the myths and beliefs that link addiction to a bad character of the addict.
“Drug addiction is unlike neurodegenerative diseases, as here the neurons are not dying. The disease is happening because of circuit dysfunction. Perhaps with different interventions, we can treat these dysfunctions,” says Christian.
Addiction remodels the fundamental mechanisms by which the brain learns and adapts to rewards. Whenever a person is exposed to a pleasurable substance, the brain attempts to form a memory of it, allowing the activity to be repeated and re-experienced.
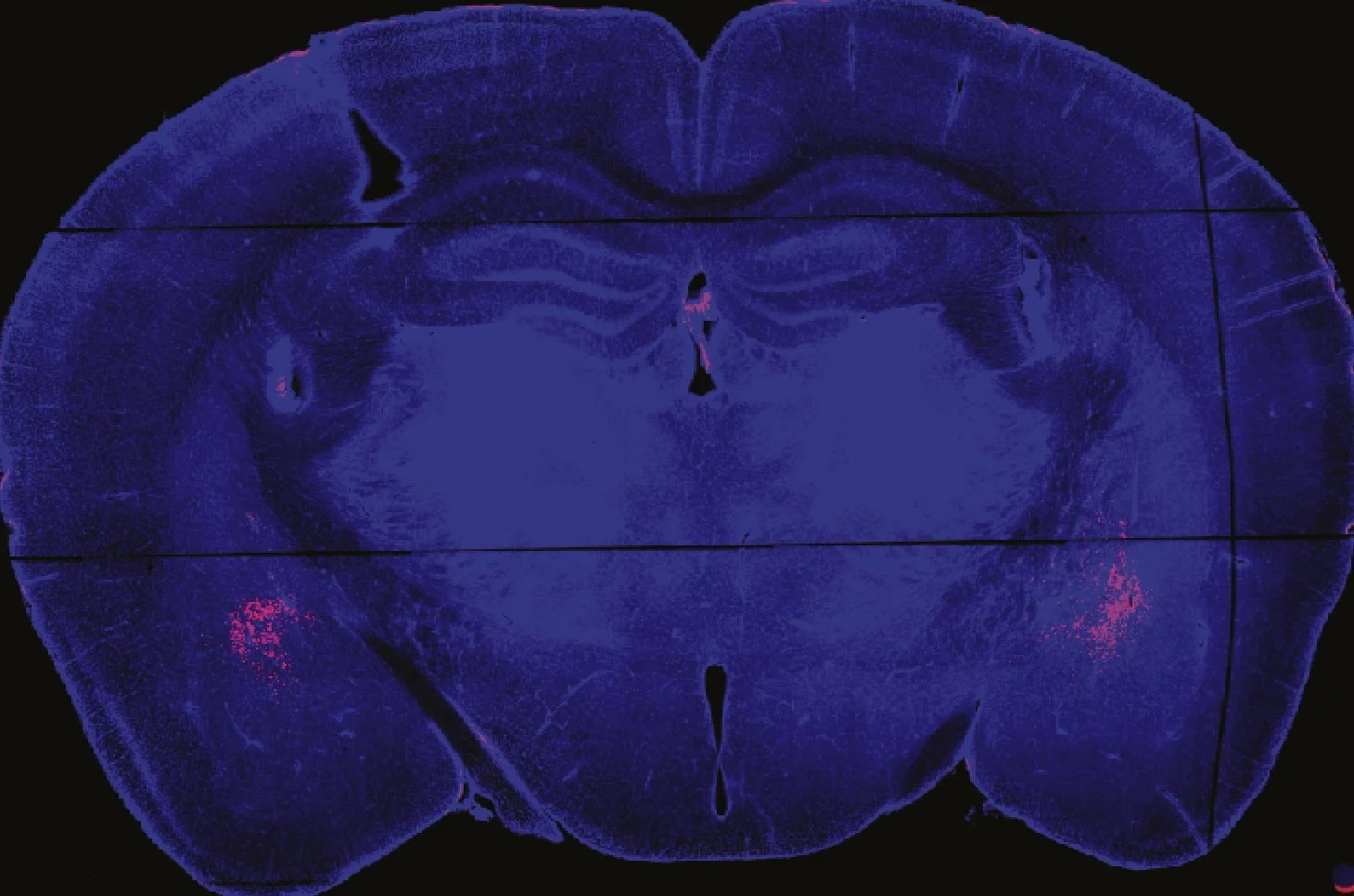
The process begins in the ventral tegmental area (VTA), where dopamine-producing neurons are activated. They release dopamine and send it to the nucleus accumbens (NAc), the brain’s reward center.
The reward center stores the memory of an action because it receives input from several other brain regions. The hippocampus provides the context of when the event occurred, the amygdala adds the emotional significance, and the prefrontal cortex records how the action was executed. Dopamine acts like a glue, favoring the binding of these neural representations together. As a result, whenever the neuron responsible for the cue fires, the neuron linked to the action is also activated, completing the circuit that reinforces the behavior.
Creating a memory of an action is like creating a trail on fresh grass. The more we walk on it, the clearer the path becomes. Similarly, the more an addictive substance is used, the more strongly the brain remembers it.
Why Some Become Addicted and Others Don’t?
However, not everyone who gets exposed to the addictive substance is predisposed to use it repetitively. A study from Christian’s lab done on a mouse model shows that while 60% of individuals may become addicts, the remaining 40% cease their use if faced with consequences, which is substantially higher than with cocaine.
His group used an interesting tool called ‘optogenetics’ that uses light to control and activate certain behaviours. By engineering dopamine-specific neurons to express the light-sensitive rhodopsin protein, scientists were able to precisely control the release of pleasure-inducing dopamine only when light was shone. Mice were provided with a lever to turn on the light, and, unsurprisingly, they pressed it so often that basic routines like sleeping and eating were neglected.
Next, the researchers decided to associate punishment with the reward. Whenever the mice pressed the lever, they received a small electric shock. As mentioned before, 40% of the individuals stopped, but the rest continued and were called the perseverers.
“The behavior observed in rodents is similar to what we see in humans. Compulsive drug use can persist even when it is associated with negative consequences. It is, therefore, important to understand what increases an individual’s vulnerability to addiction,” says Christian.
Christian’s lab uses optogenetics not only as a tool to study addiction, but also as a way to find how to reverse the addiction.
Unwiring the Brain: Reducing Compulsive Behavior
The brain learns through a process called Hebbian learning, which strengthens the connection between neurons that are repeatedly activated together. In simple terms, “neurons that fire together, wire together.”
Like unused paths that are gradually reclaimed by grass, the memory of a behavior can also fade if those neurons stop firing together. In other words, disrupting the “neurons that fire together, wire together” process can weaken the neural wiring that sustains compulsive behavior.
Mouse with a fiber-optic implant that delivers precisely timed light pulses directly into the brain. Source: Christian Lüscher
To explore this concept in practice, researchers in his lab created a protocol to reverse the addiction in mice addicted to cocaine.
Using the formidable tool of optogenetics, they found that a high-frequency burst of light strengthened the memory of cocaine addiction by causing the release of more dopamine. However, when the light flashed slowly, at intervals of every 10 seconds, the dopamine produced was insufficient to wire the neurons together. Using this method, they were able to weaken the neural connections, and the compulsive behaviors associated with addiction also subsided.
While optogenetics remains too invasive for use in humans, it holds tremendous promise for understanding and eventually reversing the neural mechanisms of addiction. For now, it serves as a powerful research tool, offering unprecedented insight into how contemporary drugs like fentanyl alter brain circuits and paving the way for future, less invasive therapies.
Addiction at the Crossroads of History, Markets, and Policy
Early this year, President Donald Trump threatened to impose punitive tariffs on China for promoting the import of fentanyl to the United States.
“Illegal market access to fentanyl is making people addicted to it. It is a painkiller, but wider access can lead to addiction, and easy access to such drugs will ensure that a certain part of the population will become addicted,” says Christian.
A recent study from his lab offers hope in this regard. They found that two different brain regions are involved in fentanyl addiction. When fentanyl is consumed, one experiences euphoria, which provides positive reinforcement, encouraging repeated use of the drug. When not consumed, the addict experiences fear and other withdrawal symptoms, known as negative reinforcement, which drives the person to seek the drug.
Previously, researchers believed that both positive and negative processes originate from a single brain region, and designed treatments like methadone to target it. The new findings suggest that µ-opioid receptors in VTA drive reward, while withdrawal stems from those in the central amygdala (CeA). This separation reveals that addiction indeed involves two independent brain pathways, opening possibilities for more targeted and effective treatments.
While the scientific community works to reverse addiction, governments should also step up to reduce the inflow and misuse of such substances. In fact, the first opioid conference in Shanghai outlawed the use of opium and morphine. A similar understanding has yet to develop around fentanyl. At the individual level, families and caregivers should also be educated about it. NGOs like Families Fighting Fentanyl actively educate and support the families and addicts to fight fentanyl addiction.
“Whenever I am invited, I like to give public talks and visit people to talk about the science I am doing because it affirms that addiction is not their moral failure,” says Christian. Scientists studying addiction have a unique power to transform despair into understanding. Such conversations should be initiated to help replace shame with empathy and silence with dialogue, reminding people that addiction is not destiny, and that healing begins with knowledge.