Looking at Alzheimer’s beyond genetics— with insights from Dr. Sivaniya Subramaniapillai
Eisha Mhatre
In recent years, Blue Zones—regions known for their high numbers of centenarians—have captured the public’s imagination, sparking interest in the science of healthy aging. While scientists have long studied how the brain ages, emerging research is uncovering early warning signs of neurodegeneration, opening doors to sooner and more effective interventions. These findings are prompting a shift in focus toward factors beyond genetics that shape brain health. As we age, the brain’s ability to adapt and form new connections naturally shifts, affecting cognitive functions such as attention and memory. While some forgetfulness, like struggling to recall a name or a past event, is a normal part of aging, more pronounced memory decline can signal the early stages of Alzheimer’s disease (AD), the most common form of dementia. In some individuals, this process is accelerated by a specific variant of the apolipoprotein E (APOE) gene, which increases their risk of developing AD. While genetics plays a role, lifestyle, nutrition, and environmental factors also profoundly influence cognitive resilience and can help reduce the risk of AD.
In our recent conversation with Dr. Sivaniya Subramaniapillai, a postdoctoral researcher at Lausanne University Hospital, she explained how behavioral and environmental factors can intersect with biology to influence AD risk as we grow older.
Sivaniya presenting at Fame Lab Swiss finals
“I’ve learned that individual life experiences, social environments, and modifiable factors like regular exercise also influence our risk for developing the disease. This insight is powerful because it shows that, while we may not be able to control the genes we’re born with, we can shape our environments and lifestyles to promote brain health and reduce our risk of cognitive decline and dementia later in life,” says Sivaniya.
Sivaniya has always been fascinated by psychology and how personal experiences, social environment, and biology come together to shape who we are. During her PhD, she came to Lausanne for an internship and enjoyed working in the FemiLab with Dr. Ann-Marie de Lange. “That experience made the transition easier because I already had a sense of what to expect. So, when the opportunity arose to continue working with the team as a postdoctoral researcher, I didn’t hesitate,” adds Sivaniya.
A recent study from Weill Cornell Medicine suggests that measuring the brain’s bioenergetic capacity—its ability to absorb and use glucose—could help detect early signs of AD in individuals at risk. As AD progresses, the brain’s ability to use glucose declines, prompting it to start utilizing alternative fuel sources, such as fats and proteins. This metabolic shift can lead to a buildup of acylcarnitines in the blood, compounds that are linked to cognitive decline and worsening AD pathology. These findings hint that maintaining a healthier bioenergetic state by potentially lowering acylcarnitine levels may shield the brain from decline.
Interestingly, gut microbiota might help in preserving bioenergetic health. In one study, elderly rats given fecal bacteria from younger rats showed signs of slower aging, including lower acylcarnitine levels. In contrast, young rats that received microbiota from older rats experienced accelerated aging. While the exact mechanisms at play here remain unclear and more research is needed to determine their relevance in humans, these findings point to a possible gut-brain connection in preserving bioenergetic health.
Along the same lines, dietary interventions that support gut health have also been shown to improve cognitive symptoms in Alzheimer’s patients by targeting key underlying pathways, such as oxidative stress and neuroinflammation. Fermented probiotics, such as kefir, are being studied for their potential to support brain health due to their unique microbial composition, which includes both bacteria and yeast. The Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diets have been linked to reduced AD risk factors, such as diabetes, obesity, and heart disease. Some studies even suggest that following the DASH diet may lower amyloid plaque buildup in the brain, a hallmark of AD. Another key, often overlooked aspect of AD is how biological and environmental factors work together to influence disease risk.
“While biology is key to understanding Alzheimer’s, lifestyle and environmental factors also play a crucial role,” says Sivaniya. “Quality sleep, regular exercise, and meaningful social engagement are essential for brain health and reducing dementia risk. But it’s just as important to recognize how our environments and social structures either support or hinder cognitive wellbeing.”
How do sex- and gender-related differences influence AD development?
We owe women centuries of research —neuroscientist Dr. Lisa Mosconi, Weill Cornell Medicine
Sex differences and societal gender norms point towards increased cases of AD in women. Image source: Adobe stock images
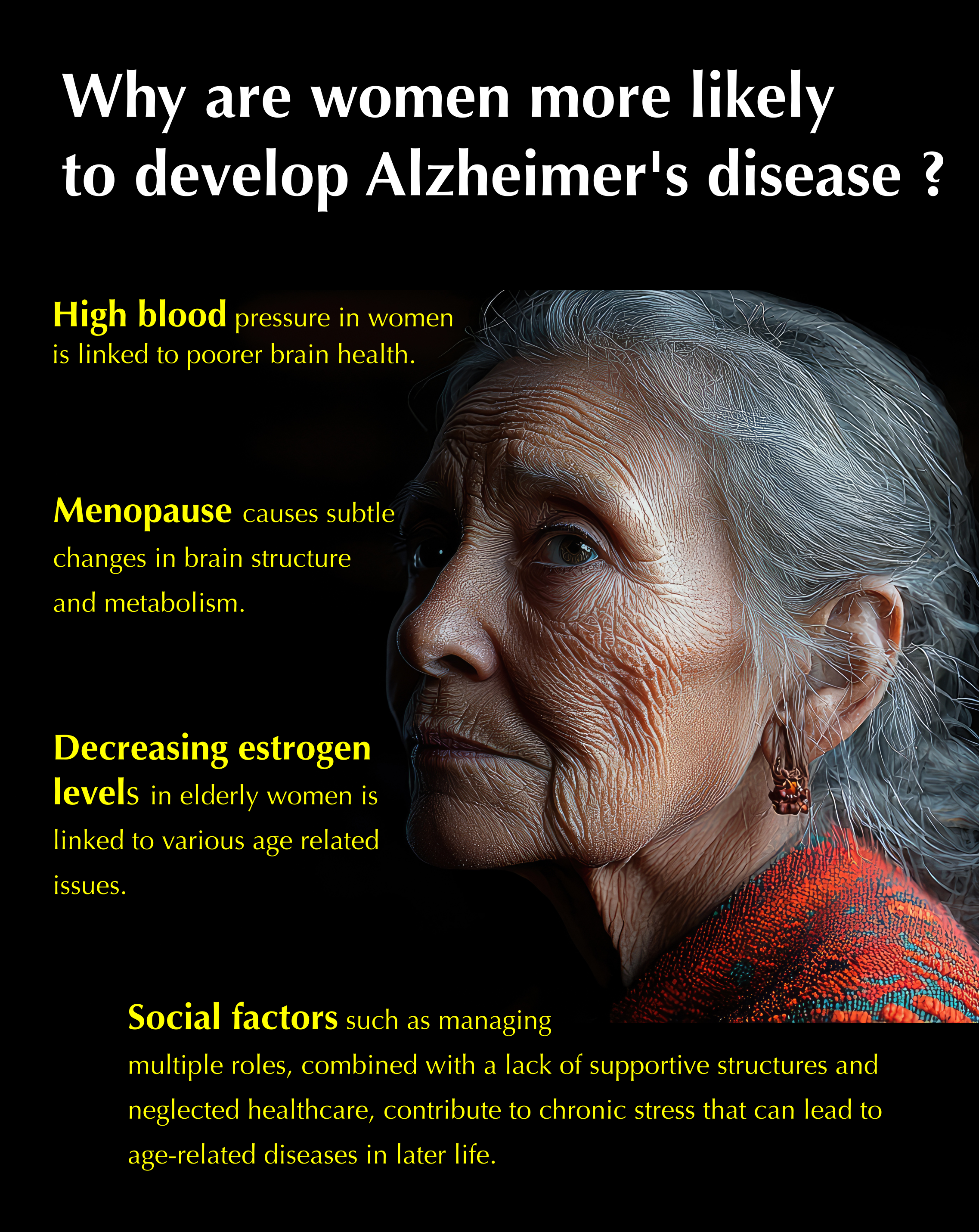
Although both men and women can develop AD, women are more frequently affected. Sivaniya’s latest research explores how heart health influences brain health differently in men and women. She and her collaborators found that high blood pressure is more strongly linked to poorer brain health in women, while in men, body weight, measured as body mass index (BMI), has a stronger link to brain health. The relationship between BMI and brain health in women appeared to be more nuanced, depending on whether or not they carried the APOE gene variant linked to increased AD risk.
A 2024 study by Arielle Crestol and Dr. Claudia Barth (also involving Sivaniya) found a complex interplay between menopause status, mental health, and genetic factors like APOE status in shaping brain health during aging in women. Menopause marks the end of a woman’s reproductive years and brings about several changes in the body, including in the brain. Research has found that menopause is linked to subtle changes in brain structure, as well as changes in brain connectivity and metabolic functions. A key factor in these changes is the decrease in estrogen, a hormone essential for energy metabolism, cardiovascular health, and brain function. As estrogen levels decline with age, women may face a greater risk of cardiovascular disease and other age-related health issues. While menopause does not automatically lead to poor health, understanding its role in aging is essential to better support women during this life stage, and may help explain their higher prevalence of AD.
But biology is only one part of the story. Sivaniya’s latest review also points to the importance of considering broader social conditions in which people age. Certain societal gender norms, for instance, can make it harder for women to engage in health-promoting behaviors beneficial to brain health. “Today, women often juggle increasing professional responsibilities with caregiving roles, which can lead to considerable stress. While caregiving itself isn’t directly linked to Alzheimer's, the chronic stress of managing multiple roles, especially without a strong support system, can contribute to a range of health issues, including age-related diseases later in life,” explains Sivaniya.
We are only beginning to uncover the complex ways sex, gender, and broader identity dimensions—like race, socioeconomic background, and culture—influence cognitive health and risk for neurodegenerative diseases. The disproportionate impact of Alzheimer’s on women of color is undeniable. These women often face intersecting challenges, including racial discrimination, limited access to education, chronic stress, and fewer opportunities for economic advancement—all of which can take a toll on brain health and cognitive function.
In her talk at the FameLab Swiss finals, Sivaniya highlighted the underrepresentation of diverse groups in brain health research, stressing the need for more inclusive approaches to both research and healthcare. “My talk focused on large-scale datasets like the UK Biobank, which is widely used—including by our team—because of its vast sample size (half a million participants!) and the wealth of available data for each individual. However, a major limitation is that approximately 96% of its participants are White, leaving just 4% to represent the nearly 20% of ethnic minorities in the UK. This raises a fundamental question: to what extent do our findings, primarily based on Western, educated populations, truly apply to underrepresented and marginalized groups?”
This lack of representation is more than a scientific oversight—it has real-world consequences. Health recommendations and interventions that are not informed by diverse data may not work as effectively for everyone.
The issue raised by Sivaniya and others in the field is urgent, especially given the rapidly growing global dementia burden. To build more inclusive science, the research community must work collectively to reduce barriers to participation and ensure broader representation in health datasets. Sivaniya points out that even within high-income countries, we must ask: “Does our sample truly reflect the diversity of the city or country where we are collecting data? If not, what barriers might be preventing broader participation, and how can we overcome them?”
Addressing these barriers and increasing diverse participation is crucial to not only improve the accuracy of our science but also ensure that the benefits of dementia research reach all communities, equitably and effectively.
If you are working on the interface between research and public health, we are interested in featuring you on this platform. Write to us.